Background: The duration of anticoagulation in patients with catheter-related thrombosis (CRT) has not been studied in a systematic fashion and is not standardized in clinical practice. Consensus guidelines have a weak recommendation for anticoagulation for 3 months after catheter removal in patients with upper extremity CRT, but this is mainly extrapolated from treatment of lower extremity deep vein thrombosis. Shorter durations of anticoagulation have been used in practice to balance the risk of bleeding and recurrent thrombosis; however, prospective data are lacking to evaluate the efficacy and safety of this practice. CRT is a frequent complication in the cancer population, who commonly requires central venous catheters for treatment. We proposed a prospective cohort study to determine the incidence of post-thrombotic syndrome (PTS), thrombosis recurrence, and bleeding in cancer patients with CRT treated with one month of anticoagulation after catheter removal.
Methods: This is a multi-institutional prospective cohort study in patients with cancer and documented upper extremity CRT. Enrolled patients were treated with a standardized protocol with therapeutic doses of enoxaparin for one month after catheter removal. Patients with platelet count <50 x 109/L, creatinine clearance <30 ml/min, history of thrombosis, or ongoing need for catheters were excluded. Demographics, catheter data, and cancer history were collected at baseline visit when catheter was removed. Incidence of bleeding, recurrent thrombosis, PTS using the modified Villalta scale, and functional limitation using the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire were assessed at months 1, 3, and 6 after catheter removal. A modified Villalta score of 5 or higher was classified as the presence of PTS and a score of 15 or higher as severe PTS. Higher DASH scores indicated worse functional disability. Binomial tests with 95% confidence intervals (CI), Skillings-Mack and Wilcoxon signed ranks tests, and Pearson correlations on log transformed values were done. Unadjusted p-values <0.05 were considered statistically significant.
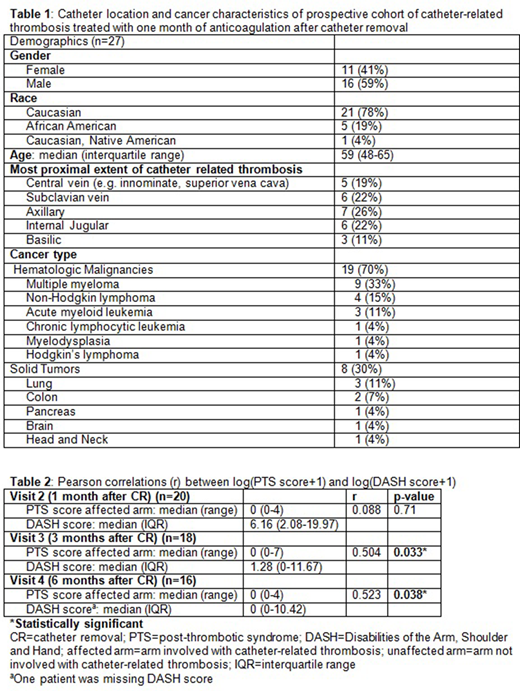
Results: Twenty-seven patients from three institutions were enrolled. Seven (26%) patients discontinued study prior to month 1, with median study duration for those who continued of 176 [interquartile range (IQR): 158-186] days. The etiologies of study discontinuation were change in therapy (n=3, 11%), requiring another catheter (n=2, 7%), bleeding (n=1, 4%), and lost to follow-up (n=1, 4%). Eleven (41%) were female, and 21 (78%) were Caucasian (Table 1). Median age was 59 (IQR: 48-65) years. The most proximal location of the veins involved with the thrombus included veins proximal to subclavian (n=5, 19%), subclavian (n=6, 22%), internal jugular (n=6, 22%), and axillary (n=7, 26%). Patients with hematologic malignancies comprised 70% (n=19) of the cohort. All patients were treated with therapeutic doses of enoxaparin for a median of 32 (IQR: 30-52) days after catheter removal. During the 6-month study duration, the incidence of recurrent thrombosis was 0% (n=0/20, 95% CI: 0%-17%), and that of major hemorrhage was 5% (n=1/20, 95% CI: 0.13%-25%). Number of patients who had at least one PTS occurrence in any visit and either arm was 15% (n=3/20, 95% CI: 3.2%-38%), and no patients had severe PTS. Higher DASH scores were associated with higher PTS scores (Table 2). DASH score differed across all visits [month 1: median 6.16 (IQR: 2.08-19.97), month 3: 1.28 (0-11.67), month 6: 0 (0-10.42), p=0.040]. Pairwise comparisons revealed that no differences in DASH scores were seen between month 1 versus 6 (p=0.44) and month 3 and 6 (p=0.098). In contrast, month 6 had significantly lower and improved DASH score compared to month 1 (p=0.0066). No deaths occurred.
Conclusions: Cancer patients with CRT frequently require central venous catheters. Treatment with anticoagulation for one month after catheter removal was associated with a low incidence of PTS, no recurrent thrombosis, and an improvement in functional disability over time in a cohort of 27 patients. The presence of PTS was associated with higher functional disability.
Baumann Kreuziger:Quercegen pharmaceuticals: Consultancy; CSL Behring: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal